Why It Matters
Findings from new UnitedHealth Group research underscore the importance of optimizing sites of care to improve patient safety and reduce costs. In particular, conducting more joint replacement surgeries in ambulatory surgery centers (ASCs) could result in 500,000 fewer hospitalizations and $3 billion in annual savings.
A Solution that Prioritizes Patient Safety
Hospital-acquired infections have long been a patient safety challenge, with 3% to 4% of hospital patients contracting infections, including infections in patients following 1% to 2.5% of joint replacement procedures. As a result, up to 26,000 joint replacement patients each year face additional treatment, longer hospital stays and potential disabilities and lost wages, while up to 800 of these patients die annually from their infections.
But many joint replacement patients do not require hospital inpatient stays. Because ASCs specialize in the procedures they perform, they can concentrate on optimizing safety and quality outcomes for patients.
ASCs with established joint replacement programs are operating safe, scalable models that achieve high-quality results for knee and hip replacement surgeries. This approach relies on specialization, repetition, scale and other key elements, including:
- Care pathways specific to joint replacement patients to help ensure each component of the surgical intervention — including pre-operative preparation and post-discharge planning — is optimally defined, sequenced and executed.
- Physicians operating with teams consisting of their preferred surgical technicians and nurses.
- Operating rooms customized for surgeons and their teams.
Surgical Care Affiliates
Surgical Care Affiliates (SCA) is a UnitedHealth Group company that operates over 230 ASCs nationwide and performs over one million surgeries each year, including joint, spine, and cardiovascular procedures. SCA offers an example of the results that can be achieved by outpatient joint replacement programs. At those ASCs performing at least 25 joint replacements in 2019, for every 1,000 patients receiving a hip or knee replacement in 2018 or 2019:
- 993 patients (99.3%) completed an infection-free surgery and were discharged without requiring a hospital visit.
- 4 patients (0.4%) required a hospital visit within 24 hours of discharge, including visits for underlying conditions.
- Fewer than 3 patients (0.3%) developed a surgical site infection.
The Savings Opportunity
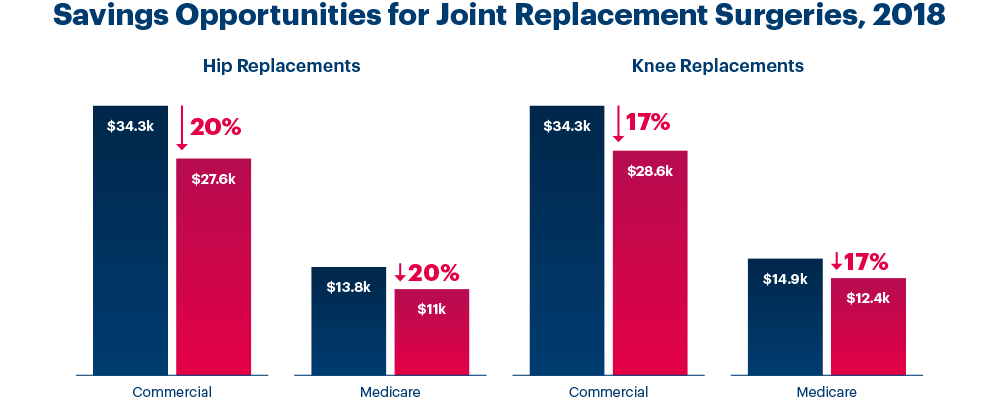
In 2019, more than 1.2 million hip and knee replacement surgeries were performed in the United States, a number that continues to rise and is expected to steadily grow over the next decade. Approximately 90% of joint replacement surgeries for privately insured individuals in 2018 took place in hospitals.
But with ASCs increasingly able to identify and treat patients more efficiently, if half of routine hip and knee replacements performed in hospitals on an inpatient basis were moved to ASCs:
- More than 500,000 surgery patients each year would avoid staying overnight in a hospital.
- $3 billion would be saved annually, including:
- $2 billion in savings for privately insured individuals and employers.
- $1 billion in savings for Medicare beneficiaries and the federal government.
Discover More
Insights & Solutions
We are committed to helping create a modern, high-performing health system and driving distinguished societal returns by improving health care access and affordability, enhancing the health care experience and achieving better health outcomes for the individuals and organizations we are privileged to serve.




Share This Story