Why It Matters
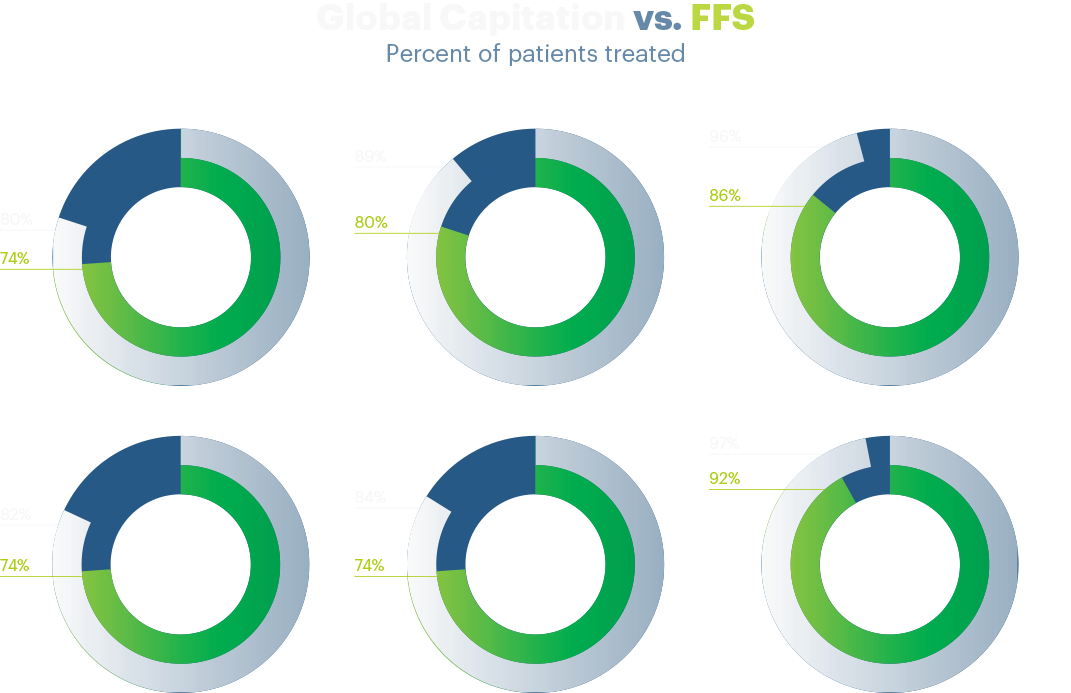
Findings from UnitedHealth Group's research underscore the importance of value-based care as a key element in building a better performing health care system for everyone. Patients benefit from global capitation because their doctors prioritize preventive care to keep them healthy and out of the hospital. Meanwhile, providers can offer valuable services that may not be paid for under fee-for-service.

Right care. Right time. Right Setting.
Primary care physicians paid under global capitation, which provides a set amount per month per patient, achieve key quality metrics at higher rates than those paid under traditional fee-for-service, according to the research. The findings indicate that capitation provides the right incentives for delivery of the right care, at the right time, and in the right setting.
UnitedHealth Group identified meaningful quality differences related to preventive care and chronic conditions using metrics from the National Committee for Quality Assurance’s Healthcare Effectiveness Data and Information Set (HEDIS).
The analysis, which reviewed more than 5 million UnitedHealthcare Medicare Advantage enrollees and tens of thousands of primary care physician practices, concluded that physicians paid under capitation are better positioned to:
- Prioritize preventive services and care management programs.
- Spend more time engaging with patients.
- Use evidence-based clinical guidance.
- Avoid unnecessary interventions on patients.
- Focus on keeping patients healthy and out of the hospital.
Commitment to Value
UnitedHealth Group has a long-standing commitment to promoting and incenting value-based care. Through UnitedHealthcare’s value-based partnerships and strong provider relationships, an increasing number of physicians are demonstrating interest in progressing to a risk-based payment model, including capitation. Optum works with providers and across the country to move from fee-for-service to value-based care, creating new choices for patients, delivering higher quality, lower cost sites of service, customizing payment models with payers, and supporting physicians to focus more on delivering care.
Today, UnitedHealthcare is working with more than 113,000 physicians and 1,200 hospitals in some form of a value-based relationship, including more than 1,250 accountable care organizations. The company’s collaboration with these providers is delivering meaningful results and better health outcomes to more than 17 million members.
Discover
Insights & Solutions
We are committed to helping create a modern, high-performing health system and driving distinguished societal returns by improving health care access and affordability, enhancing the health care experience and achieving better health outcomes for the individuals and organizations we are privileged to serve.



Share This Story